“The importance of preservation of facial function is often overlooked”
(23/9/15)
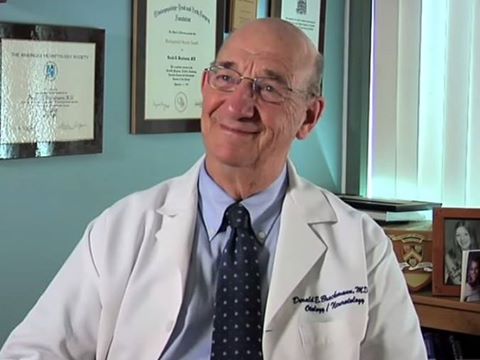
In the United States Dr. Derald Brackmann specializes in diseases of the ear, facial nerve, dizziness and acoustic neuromas (vestibular schwannomas or VS). He has served as president of the majority of the societies of his specialty, including the American Academy of Otolaryngology-Head & Neck Surgery, the American Neurotology Society, the American Otologic Society, the North American Skull Base Society and the International Skull Base Society. He is an honorary member of the Otolaryngology Society of Australia and the Royal Society of Medicine of England. He has authoring nearly three hundred scientific articles and book chapters, he is the editor or co-editor of four textbooks and is a co-editor of yearly series entitled Advances in Otolaryngology Head and Neck Surgery.1
Kind and always willing help, Dr. Brackmann accepted an interview for AMANDOS. Here, he refers to the commonest worries of NF2 patients: hearing loss, auditory implants and facial paralysis.
When did you start to feel interested in NF2? Why did that happen?
When I joined the House Ear Clinic, I was a fellow of Dr. William House. He had developed novel approaches for the removal of acoustic neuromas and had a very large practice of treating these tumors. Some of these patients had NF2 and because of the problems they encountered, I was interested in helping these patients. When the first auditory brainstem implant (ABI) was performed in 1979, that increased my interest and I became involved in that project shortly thereafter.
Which are the requirements to have an ABI or a CI (cochlear implant) placed?
A CI may be placed in certain situations in NF2. The first is if the tumor is removed and the cochlear nerve preserved, but the hearing is lost because of lack of blood supply to the cochlea. In this case, the CI may stimulate the auditory nerve. The second situation is when a tumor has been treated with radiosurgery and has remained stable. The hearing may be lost because of loss of the air cells but the cochlear nerve may still be stimulated. Some of these patients do very well. Finally, there are cases where tumors do not grow but yet the hearing is lost. These patients benefit from a CI. The ABI is done when the cochlear nerve is destroyed. In this case the CI would not be beneficial and the electrode is placed onto the cochlear nucleus in the brainstem.
When is it the best time to consider an implant placement?
The ABI is placed at the time of tumor removal. There are rare situations where it might be done without tumor removal, but we recommend it in conjunction with the surgery to remove the tumor. We recommend doing it with the first tumor removal even if there is hearing remaining on the other side. This gives the patient the opportunity to use the implant while they still have hearing in the other ear.
If an implant is placed in a patient who has been deaf for months or even years, the chances for the implant to work properly may lessen?
It is true that patients who have more recently deafened seem to perform better with implants. We have patients who have been deaf for prolonged periods of time who still benefit from either a CI or an ABI.
What do NF2 patients can expect from having an ABI or a CI placed?
Most patients that have a CI perform better than those with ABIs. Many patients with CI can hear many words without lip reading and some can even use the telephone. In general, ABIs do not perform as well. About 25% of patients will be able to understand some words without lip reading. It is very rare for them to be able to use the phone. All of the patients however have benefit in their ability to hear sounds in the environment and have improved lip reading.
If an acoustic tumor has regrown, it may damage an auditory implant?
If an acoustic tumor regrows, it could damage an ABI but usually it does not. The tumor is treated before that occurs. If there is tumor regrowth, the tumor may be removed surgically with care not to damage the implant.
Is it possible to get radiotherapy treatment if you have an implant?
Radiotherapy is the alternative. We have successfully performed gamma knife on patients with ABIs without damaging the ABI.
Does an implant can be placed if the VS have already been removed but there are tumors in any other cranial nerves?
An ABI could be placed if there are tumors on other cranial nerves that need to be removed. A large tumor on the ninth cranial nerve may obstruct the recess where the implant is placed and make that impossible. On the other hand, the tumor could be removed and an ABI placed.
Some weeks ago an article was published about the “new ABI”, how is it different from the old ABI?
Cochlear Corporation has repackaged the ABI to a thinner casing, but otherwise, it is unchanged from the prior ABI. Their performance will not be different. It should be easier to place it.
Many people in AMANDOS had had two or more surgeries to have one VS removed. We would like to know, what are the risks to have multiples surgeries to have one VS removed? Does having some residual left increase the risk of tumor regrowth?
If at all possible, we would like to do a total removable of the tumor at the first surgery. Sometimes this is impossible because of the involvement of the facial nerve or the brainstem. In that case, it is better to leave a scrap of tumor rather than injure the structures. Many of these small scraps of tumor will not regrow but if they do, further treatment may be necessary. In some cases, repeat surgery may be the best option but in others, stereotactic radiation may be preferred.
What factors affect hearing preservation during the VS removal?
The factors that affect hearing preservation are the size and location of the tumor as well as the hearing at the time of presentation. NF2 tumors must be very small in most cases in order to preserve hearing. As tumors increase in size, they involve the cochlear nerve and their removal will cause hearing loss. Small tumors that are not impacted into the inner ear canal are more favorable for hearing preservation than those that are far lateral. The best predictor of hearing preservation is the pre-operative hearing. Obviously, the better the hearing is pre-operatively, the more likely it is that it can be preserved.
If a patient has one VS instead of bilateral tumors, does treatment change?
In general, one VS would be managed much the same as our bilateral tumors. Treatment depends upon the size and location of the tumor as well as the patient’s age. Unilateral tumors are often times slower growing than the tumors of NF2. More of these tumors are observed because of that. We do believe that small favorable tumors should be removed for the best possibility of preserving hearing in either unilateral or bilateral tumors.
Are there any factors that encourage tumor regrowth?
Tumor regrowth is dependent upon the amount of tumor that is left at the time of surgery as well as the inherent biologic behavior of the tumor. Tumors in NF2 are more likely to regrow than unilateral tumors.
Is there a way to know in advance how a tumor will act out?
There is no way to predict how a tumor will behave, except that if they had rapid growth pretreatment, the tumor is likely to regrow if it is partially removed.
What is it for you the major cause of distress for NF2 patients, the risk of losing the function of the acoustic nerve or the risk of losing the function of the facial nerve?
Hearing loss is a major cause of disability for patients with bilateral acoustic neuromas, although the importance of preservation of facial function is often overlooked. Many of my patients have stated that they have overemphasized the importance of hearing in making their decision and wish that they had given more consideration to preservation to the facial nerve function.
Regarding facial paralysis, is there a way to recover the function of the nerve?
If the facial nerve cannot be preserved at the time of tumor removal, it is best to immediately insert a nerve graft. These patients frequently have good recovery of facial function. There are cases where the facial nerve cannot be found at the brainstem so a graft cannot be inserted. In those cases, some other method of restoration of facial nerve function must be sought. One option is to do what is called a partial hypoglossal facial nerve anastomosis. In this surgery, a portion of the nerve which supplies motion to the tongue is connected to the facial nerve. This procedure will restore good facial tone and some motion that is a big improvement over the total facial paralysis. Other techniques include connecting one of the nerves that goes to the chewing muscle to the facial nerve and in some cases, a nerve graft from the other unaffected side can be placed to the facial nerve on the paralyzed side. Other techniques include muscle grafts and muscle transfers.
If surgery is needed, is it advisable to try Avastin first?
Avastin can be very helpful in arresting tumor growth and preservation of hearing in some patients with NF2. If patients have growing tumors with preserved hearing, Avastin can slow the tumor growth and preserve hearing for a long time. This is advisable in these cases. This must be managed by an oncologist as there are complications to Avastin treatment. It has been a significant help in the management of patients with NF2.
Do you know if some research is being done with genetic therapies to restore hearing in deaf people with NF2?
There is considerable research being done on different drug therapies for arresting the growth of tumors in NF2. I am unaware of any genetic therapies to restore hearing in deaf people with NF2.
Interview: Norma Ortiz for AMANDOS
